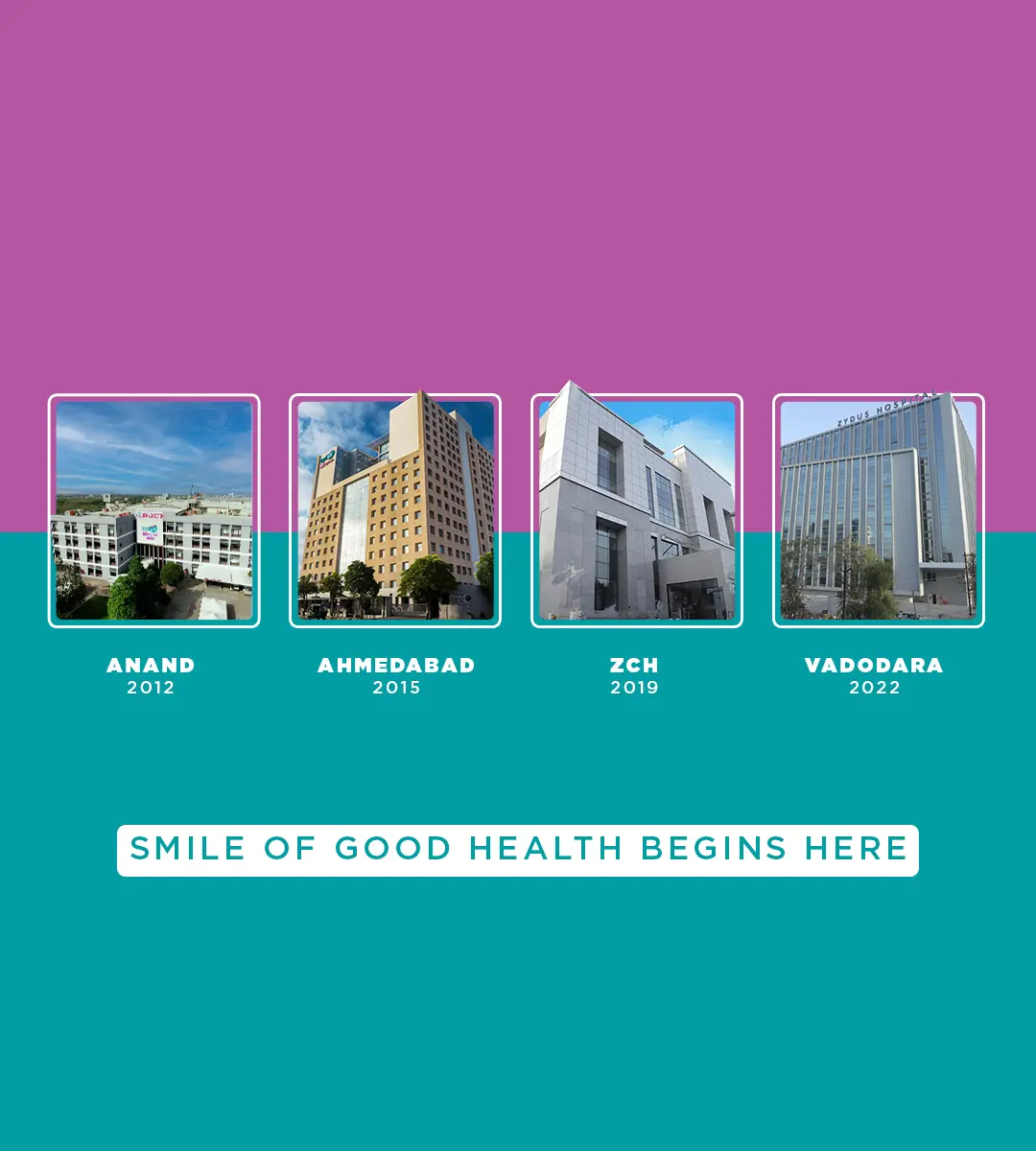
Zydus Hospitals
Multispeciality Hospital OF GUJARAT
A Complete Hospital
THE BEST MULTISPECIALITY HOSPITAL OF GUJARAT crowned with trust, brings to the table a class of its own.
Making the healthcare group a key player in keeping Western India ahead of the curve, Zydus Hospitals has the mission to extend World Class healthcare solutions to the community through advances in medical technology & research. By adopting best man management practices - Zydus Hospitals has benchmarked its existence in the state of Gujarat. Offering the best of medical facilities, it stands being Western India's largest private hospitals.
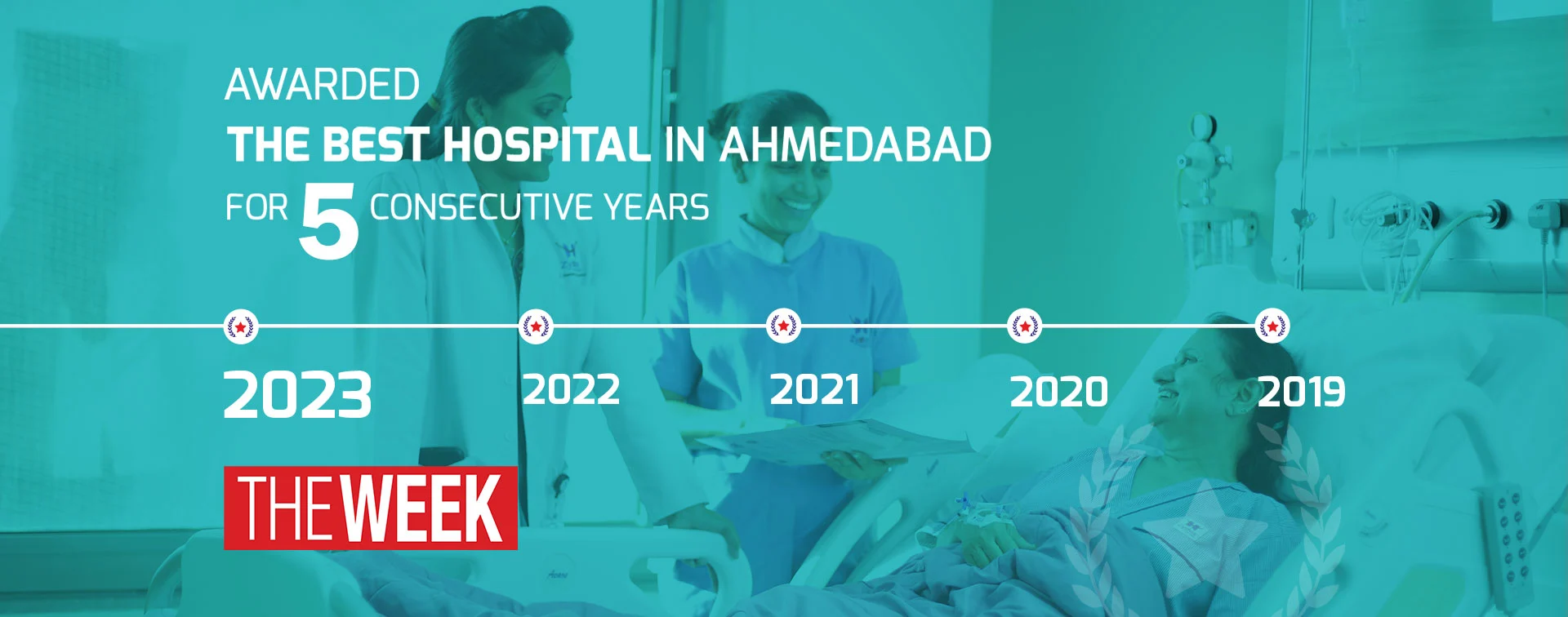
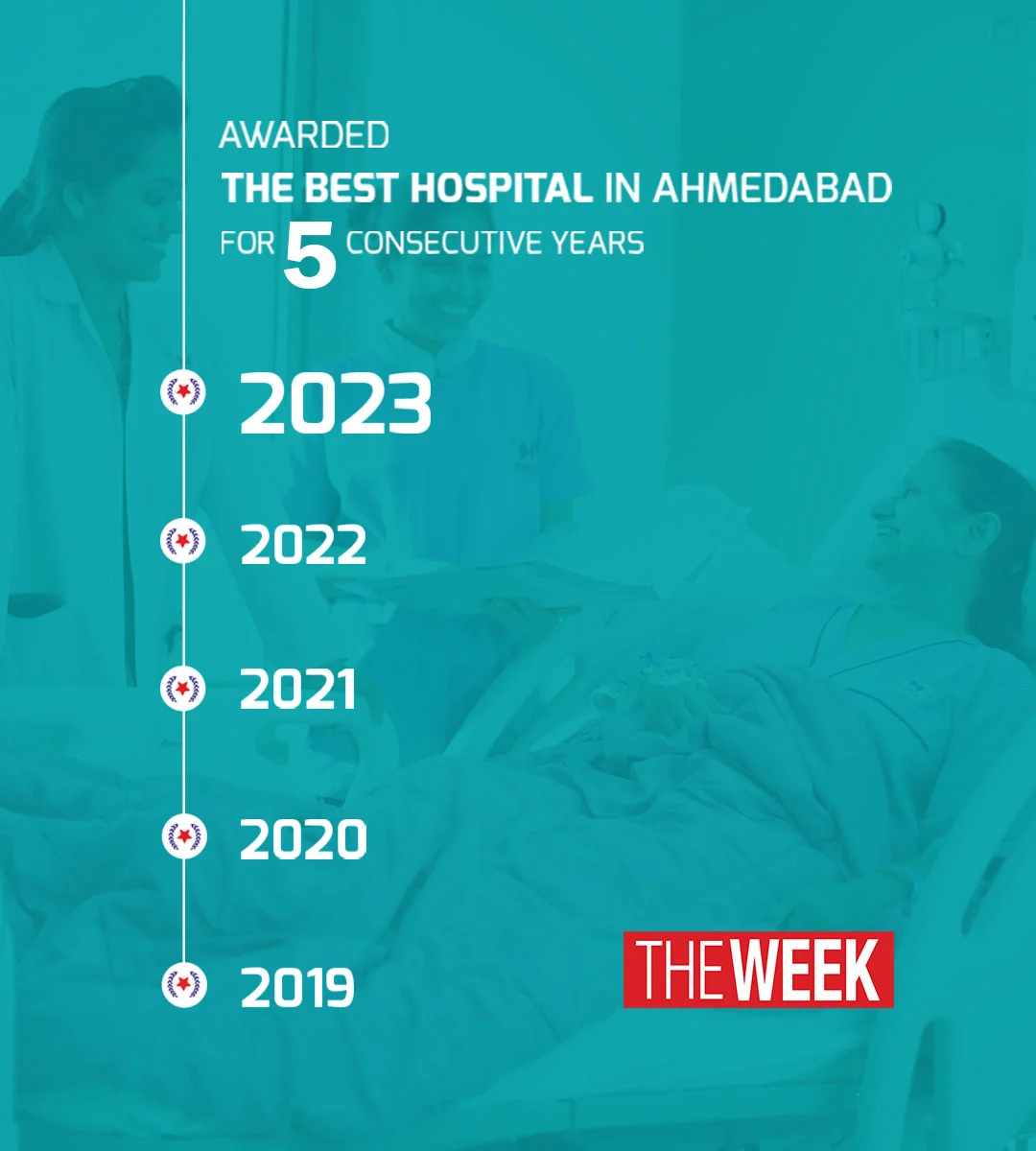
ZYDUS HOSPITALS AND HEALTHCARE RESEARCH PRIVATE LIMITED has been striving to create milestones of recovery stories since inception. We have been restoring hope and health while being recognized for sheer dedication, precision, excellence and selfless service. Whether it is about our sound infrastructure, patient-centric approach, team of experts, management, medical facilities, cutting-edge technology, coordinated care, transparent pricing or emergency services, we have been constantly receiving words of appreciation.
Accreditation





Clinics
Heart Rhythm Clinic
- A good heart beats regularly. Irregular heartbeats are grounds for concern. At the Heart Rhythm Clinic, get the finest advice from our specialists to ensure that your Heart functions normally.
Brain Stroke Prevention Clinic
- Prevention is better than Cure. More so, with Brain Strokes. At the Brain Stroke Prevention Clinic, patients are assisted with proper assessment of risk factors, corresponding lifestyle changes, and adapting healthy habits.
Heart Failure Clinic
- An improperly functioning heart can lead to blood backing up and causing fluids to build up in Lungs and Legs. This build up can cause breathlessness. This can lead to heart failure and can be fatal. At the Heart Failure Clinic, we take care of the heart muscle and in turn its pumping capacity.
Allergy Clinic
- Allergies are painful. And going to allergy clinics, is scary. At our Allergy Clinic, with a single serum sample, we detect around 300 allergens. This in turn helps to identify the agents triggering the allergy, making the process comfortable and treatment easier.
Fertility Clinic
- Becoming Parents is the biggest joy that many couples dream of. Not being able to conceive naturally, can shatter those dreams. At our Fertility clinic, with an advanced scientific approach, we work towards making the parenthood a reality for such couples.
Pain Clinic
- Managing pain is a task in itself. Especially healthcare pains which can be acute, chronic and challenging. Our specialized Pain Clinic devises pain management plans for Back, Knee, Hips, Cancer, and many more – making it easier for the patients.
Sleep Disorder Clinic
- A sound sleep is essential for good health. Sleep disorders can get your life into disarray. This needs to be addressed by testing and monitoring Sleep Apnea. Our Sleep Disorder Clinic does this by running a test that monitors heart, lungs, and brain activity. It also monitors breathing patterns, arm & leg movements, and blood oxygen levels when one is asleep.
Aesthetic Surgery Clinic
- Looking good is no more only natural or being lucky - modern day cosmetic surgeries at our Aesthetic Surgery Clinic offers Tummy Tucks (Abdominoplasty), Breast Augmentation, Breast Reduction, Eyelid Surgery, Nose Reshaping (Rhinoplasty), Face Lift and Liposuction (Removal of fat) - to enable patients to look stunning.
Skin & Hair Clinic
- Hair and Skin are the final additions to good looks. Our Skin and Hair Clinic, by treating skin and hair issues, tops one’s good looks and complements the efforts of our Aesthetic Surgery Clinic, and even more.
Fever Clinic
- Fever is considered the simplest indication of getting unwell. If not detected correctly, or on time, it can become dangerous. We have a specialized Fever Clinic to diagnose from simple seasonal flu to paediatric flu, to Malaria & Dengue, and even Covid-19. Don’t take fever lightly.
Zydus Juniors
- A child’s health is the most crucial part in any family and we understand that. At Zydus Juniors, we have a team of leading & expert Paediatricians who not only treat children with acute or chronic illness, but also advise parents on preventive healthcare to ensure a healthy childhood.
Zydus Moove
- Physio issues are becoming a regular part of our lives. Accidents, damages, lack of vitamins, etc. can pose challenges for normal movements. At Zydus Moove, we ensure that the patients receive most appropriate Physiotherapy as per every situation.
Liver Clinic
- Liver is a vital organ. Needless to say, any issue related to Liver needs to be taken seriously, and addressed accordingly. Liver problems can lead to Jaundice, Viral Hepatitis – A, B,C,D,E, Cirrhosis (Liver Failure), Enlarged Liver, Hepatic Encephalopathy, Ascities fluids in belly, and also to Tumour in the Liver, or Cancer. Timely diagnosis, and proper treatment can be lifesaving. Zydus Liver Clinic offers the patients exactly that, with its accurate treatment.
Joint & Bone Clinic
- Changing lifestyle and food habits can result into Joint Pain. Sports injuries, fractures, and trauma injuries are also increasing. Our Joint & Bone clinic addresses all these issues, including Ostero Arthritis, with help from our finest experts.
Sexual Dysfunction Clinic
- Sexual problems are real - not to be hidden, but treated properly. Difficulty in sexual response, in having orgasms, or having pain during intercourse – these problems need help from experts. Our expert Urologists at the Sexual Dysfunction Clinic are there to help those suffering lead a satisfied, and happy life.